Stem cell therapy for sports injuries gives athletes a non-surgical option to reduce pain, support tissue repair, and speed a safe return to play by harnessing the body’s biologic repair signals. This guide walks through what stem cell therapy is, how it helps common athletic injuries, and the main approaches used by clinics in San Antonio — including mesenchymal stem cell (MSC) therapy, bone marrow aspirate concentrate (BMAC), and umbilical cord–derived stem cell treatments. Many active patients are frustrated by lingering pain, slow healing, or surgeries that demand long rehab. Modern regenerative orthopedics can offer targeted alternatives that prioritize restoring function and limiting opioid use. Below we define the treatment and mechanism, review injury-specific applications (knee, shoulder, hip, tendon), compare stem cell care to surgery and medication, outline realistic recovery timelines, and explain how to schedule a consultation with a qualified stem cell doctor in San Antonio clinic. Throughout, we focus on practical, evidence-based guidance and clear next steps so athletes can make informed choices about regenerative options.

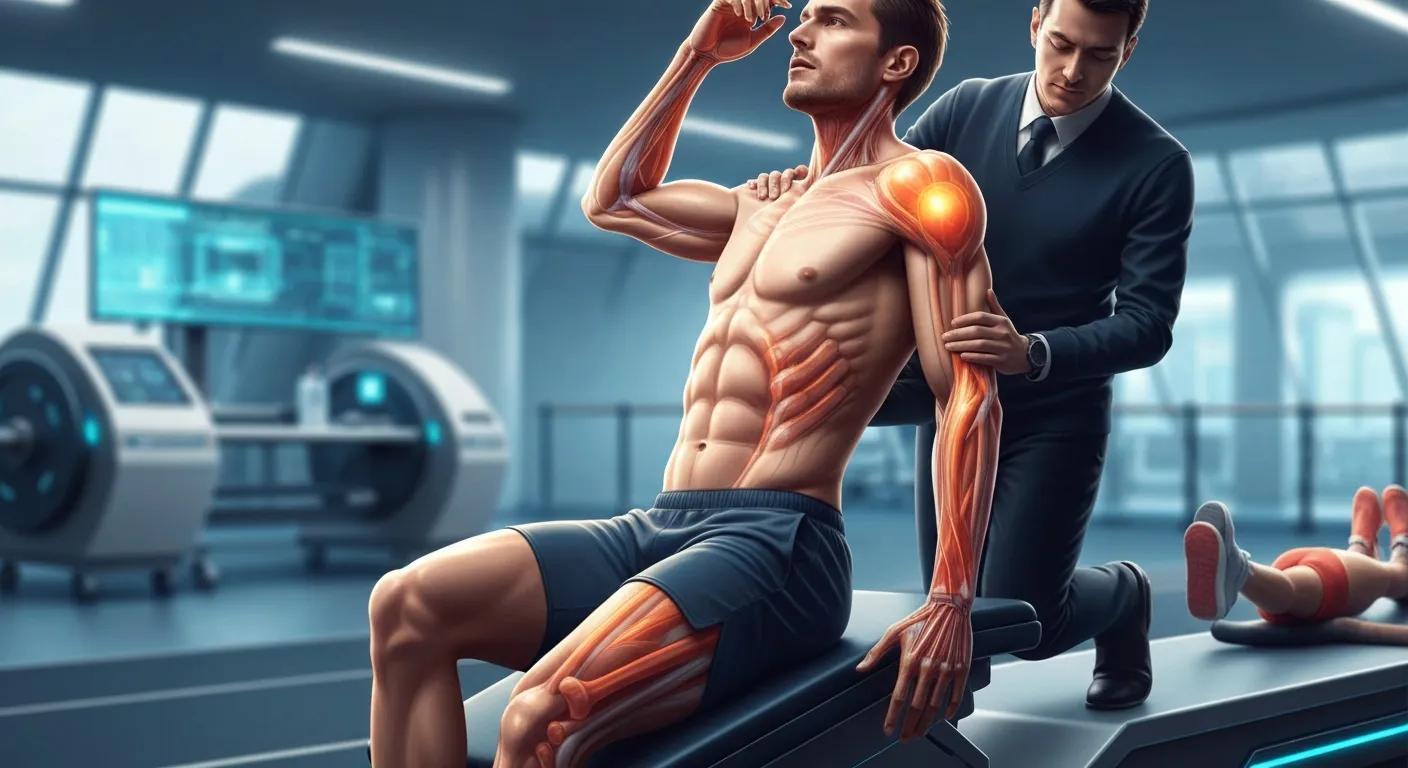
Stem cell therapy for sports injuries is a branch of regenerative medicine that uses living cells or cell-derived factors to reduce inflammation, support tissue repair, and relieve pain in musculoskeletal problems. The primary actions are anti-inflammatory signaling and paracrine factor release from therapeutic cells, which encourage local repair processes and can support collagen remodeling in tendons and preservation of cartilage matrix in joints. For athletes, the key advantage is targeted biologic support that complements rehabilitation and—when appropriate—can reduce the need for invasive surgery. Recent studies through 2023 highlight that careful treatment selection, precise injection technique, and imaging guidance affect outcomes, and that adjunct therapies can improve results.
Stem cell therapies are one tool in a broader regenerative orthopedics toolbox that includes platelet-rich plasma (PRP), shockwave therapy, and other advanced modalities designed to optimize healing. Knowing how different stem cell sources differ helps athletes and clinicians choose the right option for each injury. The sections that follow explain the biology and summarize the main treatments available locally in San Antonio.
Stem cell therapy promotes healing mainly through immunomodulation and paracrine signaling rather than by simply replacing damaged tissue. Therapeutic cells—especially mesenchymal stem/stromal cells (MSCs)—release growth factors and cytokines that lower inflammation, recruit native repair cells, and stimulate extracellular matrix synthesis in tendon and cartilage. In short: therapeutic cells → release paracrine factors → reduce inflammation and encourage regeneration. Image guidance such as ultrasound or fluoroscopy helps place injections precisely into the injured structure, increasing biologic effect while minimizing trauma to surrounding tissue.
Clinically, biological treatments deliver the best results when combined with a structured rehabilitation program. The biologic creates a window for tissue remodeling; rehab translates that biologic change into lasting strength and function. Evidence through 2023 shows meaningful symptom reduction in many tendinopathies and early degenerative joint conditions when cell therapies are selected appropriately and paired with physical therapy. With that foundation, we’ll review the common stem cell sources and why one may be chosen over another.
San Antonio clinicians typically use three broad stem cell approaches for athletic injuries: mesenchymal stem cell (MSC) therapy, bone marrow aspirate concentrate (BMAC), and umbilical cord–derived stem cell therapy. Each source differs by origin, typical indications, and regulatory/processing considerations: MSCs can be harvested from adult tissues and are used for their anti-inflammatory and regenerative effects; BMAC is an autologous marrow concentrate often selected for focal tendon and cartilage repairs; umbilical cord tissue provides an allogeneic, growth factor–rich option with extracellular matrix components. Complementary therapies such as PRP, shockwave therapy, and Class IV laser are frequently combined to support healing.
This comparison clarifies why clinicians select different modalities based on injury type, chronicity, and the athlete’s goals. Injection technique and rehabilitation are then tailored to get the most from the chosen therapy.
Stem cell therapy can help a variety of sports injuries—particularly cases with inflammation, partial tissue loss, or degenerative change where reconstruction isn’t mandatory. Common targets include tendon and ligament problems, focal meniscal or cartilage defects, partial rotator cuff tears, labral irritation, and early degenerative joint disease. The primary goal is to reduce inflammation and support matrix repair so athletes can regain pain-free motion and functional performance when treatment is combined with a structured rehab plan.
Knowing these injury-specific considerations helps athletes choose the right path instead of defaulting to surgery. The next sections outline knee, shoulder, and hip applications in more detail.
For knee injuries, regenerative injections are generally used for partial structural injuries, meniscal tears amenable to conservative repair, and early cartilage degeneration when joint preservation is the goal. For example, focal meniscal tears that cause symptoms can be managed with targeted biologics, offloading strategies, and progressive rehab to reduce inflammation and support tissue integration. Return-to-play is guided by injury severity, sport demands, and objective functional testing—not by fixed timelines; some athletes return to modified training within weeks and to full competition after gradual progression over months.
Adjuncts such as PRP or shockwave therapy are commonly combined with stem cell approaches to boost local growth factor availability and encourage tendon remodeling. A rehab plan that advances from protected range-of-motion to strength work and sport-specific drills is essential to turn biologic changes into durable performance gains.
In shoulder and hip conditions, stem cell therapy aims to reduce pain, improve range of motion, and support tissue healing for issues like partial rotator cuff tears, tendonitis, and select labral irritations. Biologic treatments can lower local inflammation and promote more organized collagen in tendons, translating to better load tolerance and less dependence on pain meds. Athletes often regain mobility and functional strength faster when biologic care is paired with a progressive, sport-specific rehab program that restores shoulder or hip mechanics.
Selecting biologics for shoulder or hip care requires a clear assessment of structural integrity; full-thickness tears or major instability may still require surgery. For appropriate candidates, regenerative approaches can shorten symptomatic periods and support a gentler, tissue-focused return to sport.
Choosing a stem cell clinic means evaluating treatment options, safety practices, and the care pathway that supports your return to sport. NexGenEsis Healthcare’s San Antonio team emphasizes non-surgical, narcotic-sparing pain relief and a personalized care model that pairs regenerative procedures with targeted rehabilitation. Our practice offers core stem cell services—MSC therapy, umbilical cord stem cell therapy, and BMAC—along with complementary regenerative tools like PRP, shockwave therapy, Class IV laser, A2M injections, and peptide-assisted recovery to build individualized protocols for each athlete.
Our clinic-centered pathway ensures treatment choices match your injury, sport demands, and timeline rather than applying one-size-fits-all solutions. When comparing local providers, these value points help you evaluate care philosophy and rehab support.
Our clinicians blend sports medicine expertise with regenerative orthopedics to ensure careful patient selection and precise procedural technique. Their competencies include focused musculoskeletal assessment, image-guided injection skills, and a working knowledge of biologic product attributes to match therapy to tissue pathology. That structured sequence—assessment, imaging, targeted biologic delivery, and progressive rehabilitation—creates continuity that improves the chances biologic effects translate into real functional gains.
Focusing on clinical skill sets rather than isolated credentials helps athletes evaluate the care model: advanced image-guided injections, evidence-informed therapy selection, and coordination with physical therapy all support better outcomes. That clarity leads to more realistic expectations about treatment pathways and recovery timelines.
At NexGenEsis we begin with a detailed assessment and imaging to identify the tissue pathology and biomechanical contributors to your injury. From that base we design a multimodal plan that may combine MSC, BMAC, or umbilical cord therapies with PRP, shockwave, or Class IV laser to optimize the local healing environment. Rehabilitation is integrated from day one, with phased progressions that align biologic healing windows to strength and neuromuscular retraining so athletes regain lasting function.
This patient-centered sequence—assessment → targeted biologic therapy → structured rehab—prioritizes non-surgical pain relief and minimizes narcotic reliance by focusing on biologic modulation and functional restoration. For athletes who want to reclaim movement and return to competition, our approach balances regenerative science with practical recovery planning.
Stem cell therapy differs from traditional care by aiming to support biological healing instead of only managing symptoms or mechanically reconstructing tissue. Compared with surgery, regenerative injections are less invasive, carry lower immediate procedural risk, and often allow faster early recovery; still, surgery remains the standard when mechanical reconstruction is required. Compared with medication, stem cell therapy seeks to alter the disease process—reducing inflammation and encouraging matrix repair—rather than only masking symptoms.
The table below summarizes tradeoffs to help you weigh stem cell therapy against surgery and medication-based approaches.
For properly selected athletes, non-surgical stem cell therapy offers clear advantages: lower procedural risk, less reliance on narcotics, and the potential for biologic tissue repair rather than only symptom control. By modulating inflammation and stimulating matrix synthesis, these approaches can improve function while preserving native anatomy—especially valuable for athletes who want to minimize downtime. Pairing biologics with structured rehab also lets us address biomechanics and muscle deficits that raise re-injury risk.
Those advantages must be balanced with limitations: not every injury is appropriate for non-surgical care, and evidence varies by indication. Individualized assessment is essential.
Stem cell therapy can shorten symptomatic recovery in many cases by reducing pain and creating a biologically favorable environment for repair. Performance gains, however, depend on comprehensive rehabilitation and sport-specific conditioning. The relationship is straightforward: biologic therapy → reduces inflammation and supports matrix repair → creates a rehabilitation window for strength and neuromuscular retraining. Return-to-play timelines therefore depend on biologic response plus the quality and progression of rehab.
Realistic expectations matter: some athletes experience faster symptom relief and functional gains, but lasting performance improvement requires targeted training to rebuild sport-specific strength and technique. Clinicians emphasize progressive load management and objective testing to ensure a safe transition back to competition.
Expect a staged process: a diagnostic evaluation with imaging, a tailored treatment plan that specifies the chosen biologic approach and procedural details, and a rehabilitation timeline. Procedures are typically performed under local anesthesia with image guidance and last roughly 30–90 minutes depending on complexity and adjuncts. Immediately after the procedure you may have temporary soreness and activity limitations; medium-term recovery focuses on graded loading and measurable functional milestones over weeks to months.
Before treatment we review realistic goals and consent based on current evidence through 2023, including variability in outcomes. Follow-up visits track pain, function, and objective measures to guide progression. The practical steps below illustrate the typical path from consult to return-to-play.
This stepwise pathway helps athletes prepare mentally and practically for recovery while emphasizing measurable progress.
Recovery varies by injury type, the tissue being treated, and athlete-specific factors like age and metabolic health. Immediately after an injection expect localized soreness for a few days and activity limits for one to two weeks to let the biologic settle. Functional improvements typically appear over weeks to months as tissue remodels—tendon remodeling and progressive strength gains often emerge in 8–12 weeks, while cartilage-related benefits may take several months under structured load management.
Rehab milestones guide progression from protected range-of-motion to strengthening and sport-specific drills; objective testing determines readiness for full competition. Because timelines differ, clinicians favor individualized plans rather than fixed return-to-play dates to balance safety and performance.
When performed by trained clinicians with sterile, image-guided technique, stem cell procedures have a low rate of complications. Common, usually short-lived effects include injection-site pain and localized swelling; rare but possible risks include infection or procedural complications that proper protocols aim to prevent. Success rates depend on the indication, injury chronicity, the biologic used, and the rigor of rehabilitation. Reviews through 2023 report symptomatic improvement for many tendinopathies and early degenerative joint conditions, but outcomes are variable and hinge on careful candidate selection.
Factors that influence success include injury type, timing of intervention, the chosen biologic product, and adherence to a structured rehab program. Transparent, evidence-based consent and realistic goal-setting help athletes understand likely benefits and limitations.
To schedule a consultation, be ready to summarize your injury history, prior treatments, and performance goals so clinicians can assess candidacy for regenerative options. A typical consult includes a clinical exam, imaging review, discussion of treatment choices and timelines, and a personalized plan that incorporates rehab. Costs and insurance coverage vary, so clinics usually provide individualized estimates after clinical review and can discuss financing options when appropriate.
To start a consult with a San Antonio specialist, use the clinic’s San Antonio location page or its verified business listing to request an appointment or a virtual pre-screen. Bring prior imaging and a clear statement of your sport demands—this helps the care team create an efficient, focused plan. The table below summarizes service steps, what each includes, and typical next steps to clarify scheduling.
Costs vary widely depending on the therapy type, number of sessions, and adjunct services. Many regenerative procedures remain out-of-network for standard insurers and require self-pay or supplemental coverage. Because pricing depends on the chosen protocol and products, clinics typically provide a personalized estimate during the consultation that covers imaging, the procedure, and follow-up rehab. Athletes should check their plan’s coverage for injection procedures and ask clinics about available financing to plan accordingly.
Because costs vary, request a detailed estimate at your initial consult so financial expectations align with the recommended treatment pathway. Open discussion early in the process reduces surprises and helps you weigh benefits against your sport timeline and goals.
To reach the San Antonio regenerative team, visit NexGenEsis Healthcare San Antonio or use the clinic’s verified online listing to request an appointment or virtual evaluation. When you contact us, provide prior imaging, a concise injury history, and your athletic goals so the care team can prepare focused recommendations. We offer in-person evaluations and remote pre-screening to determine candidacy and plan the most efficient in-office procedure day.
Stem cell therapy is generally safe when performed by experienced clinicians under sterile, image-guided technique. Common short-term effects include injection-site pain and swelling or temporary increased discomfort. Rare risks include infection or procedural complications—risks that careful technique and protocols minimize. Discuss your specific risk profile with your provider so you understand what to expect.
Costs vary widely by treatment type, number of sessions, and clinic. Upfront expenses for stem cell therapy are often higher than for medication or basic physical therapy, but many athletes find potential benefits—faster recovery and reduced need for surgery—make it cost-effective over time. Ask about a detailed estimate and financing options during your consultation to understand the full financial picture.
Yes. Stem cell therapy can be effective for chronic injuries that involve inflammation or degeneration, such as tendinopathy and early osteoarthritis. Success depends on the specific condition, timing of treatment, and a complementary rehab program. A specialist evaluation will determine whether regenerative therapy is a good fit for your chronic issue.
Rehabilitation is central to maximizing treatment benefits. A structured rehab plan aligns with the biologic healing process and progresses from range-of-motion to strength and sport-specific drills. Effective rehab not only improves recovery but also reduces re-injury risk by addressing movement patterns and strength deficits. Work closely with your rehab team to get the best outcome.
Individual timelines vary. Many athletes notice pain and function improvements within a few weeks, but full benefits often take several months as tissues remodel. Tendon healing commonly shows clear gains around 8–12 weeks; cartilage-related improvements can require longer. Regular follow-ups let clinicians track progress and adapt rehab as needed.
Stem cell therapy is not appropriate for every injury. Severe structural damage—complete tears or major joint instability—typically requires surgical repair. Active infections, certain medical conditions, or specific contraindications may also preclude treatment. A thorough specialist evaluation determines whether stem cell therapy is a safe and sensible option for your case.
Stem cell therapy gives athletes a promising non-surgical option to reduce pain, enhance recovery, and restore function for many sports injuries. By working with the body’s biologic repair processes, regenerative care can reduce medication reliance and help speed return-to-play when paired with the right rehabilitation. Understanding the available options in San Antonio empowers athletes to choose the path that fits their goals. Schedule a consultation to learn whether stem cell therapy can support your athletic comeback.