Stem cell therapy follows a predictable, phased biological course: early anti-inflammatory effects appear first, then months of gradual structural repair. That means most patients see steady improvement rather than an instant cure. This guide explains when you can expect pain relief, how strength and mobility typically return over weeks to months, and what longer-term remodeling looks like for joints, nerves, and soft tissues. If your question is, “How long until I notice results?” — this article gives condition-specific timelines, practical rehab tips, and evidence-aligned expectations. You’ll learn the Immediate, Incubation, Regeneration, and Long-term phases; the main factors that speed or slow recovery (age, severity, cell source); and expected timing for knee osteoarthritis, nerve repair, and sports injuries. Throughout, we highlight how adjunct therapies and patient behaviors influence outcomes and describe the clinical milestone framework our teams use to set realistic next steps.
Ready to explore personalized stem cell therapy options? Schedule a consultation with our expert stem cell doctors at NexGenEsis Healthcare San Antonio to discuss your unique healing journey.
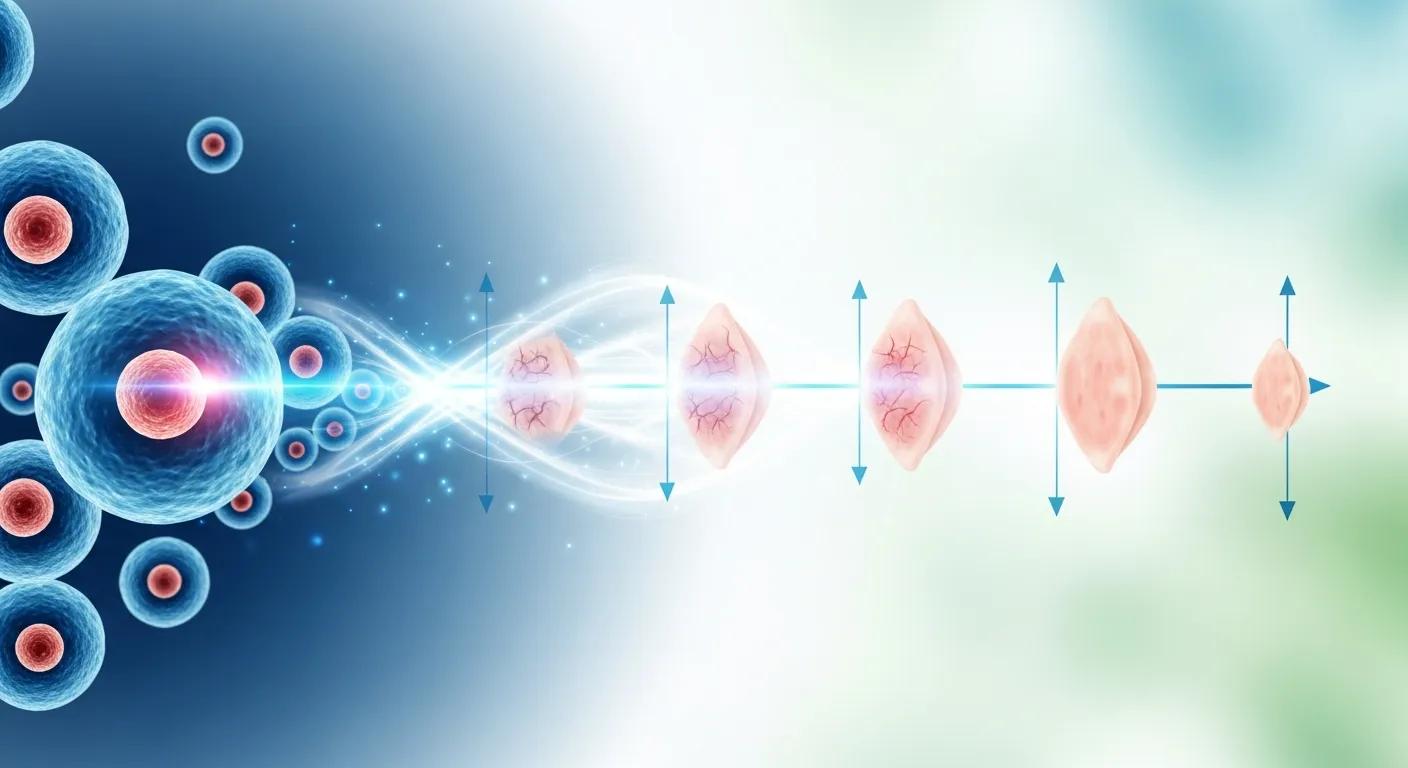
We commonly describe the healing process in four overlapping windows: Immediate (days 1–7), Incubation (weeks 2–4), Regeneration (months 2–6), and Long-term remodeling (6+ months). Early improvements most often reflect anti-inflammatory and paracrine signaling that reduce pain and swelling. Later gains come from tissue repair and remodeling as stem cells, and their secreted factors support healing. Knowing these windows helps you track progress and avoid premature conclusions, since measured functional improvement often follows symptom relief. The section below translates those biological windows into practical expectations so you know what to watch for and when to contact your provider.
The timeline below gives concise numeric windows to set realistic expectations.
These stages create a useful roadmap for tracking recovery and planning rehab or adjunct treatments. The next subsection explains how early biological effects produce the first signs of improvement.
Early healing after stem cell therapy is driven mostly by paracrine signaling and anti-inflammatory effects rather than immediate tissue replacement. Many patients notice symptom relief within days to a few weeks. Clinical observations show factors released by mesenchymal stem cells can lower local inflammation and pain signaling, often reducing pain medication needs and improving sleep in the first 1–6 weeks. Those early changes can be modest and sometimes ebb and flow as the immune environment adapts, so we advise tracking pain and function over time rather than judging progress on a single day. Recognizing that early relief represents biological signaling — not structural repair — helps you prepare for the later regeneration phase when true tissue healing becomes evident.
Recovery after injections follows recognizable stages that line up with symptom patterns and functional milestones. The Immediate stage (days) brings anti-inflammatory benefit and localized soreness. The Incubation stage (weeks) involves cellular homing and variable symptoms. The Regeneration stage (months) delivers measurable improvements in strength and motion. Finally, the Long-term stage (six months plus) focuses on consolidation and maintenance. During regeneration, many patients reduce their reliance on pain meds and tolerate more daily activity; higher-level tasks return later as tissue strength improves. Knowing these stages helps you plan rehab and set realistic goals with your provider.
How quickly and how fully stem cell therapy helps depends on a mix of patient, condition, and procedural factors. Key influencers include age and overall health, how advanced the condition is, the stem cell source used, adjunct treatments like PRP or shockwave, and adherence to post-procedure rehab. Clinicians weigh these elements when estimating your timeline and suggest optimizations to improve outcomes. The table below summarizes common factors and their typical effects on onset and magnitude of improvement.
This overview shows how each factor changes expectations and supports individualized planning. The list below highlights the most impactful modifiers clinicians consider when estimating timelines.
Understanding these factors leads into practical steps patients can take to support faster recovery.
Biological age and systemic health strongly influence regenerative capacity. Chronological age is only part of the story — metabolic health, circulation, and inflammation control matter most. Younger patients with good cardiovascular fitness and well-managed metabolic markers usually mount stronger repair responses. Conditions like diabetes and smoking harm microcirculation and slow cell-mediated repair. Clinicians commonly recommend optimizing nutrition, controlling blood sugar, quitting smoking, and correcting vitamin deficiencies to improve both the speed and durability of gains. These are actionable steps that often make a meaningful difference.
The type of tissue and how advanced the damage is are major drivers of timeline differences. Early-to-moderate cartilage lesions in the knee often respond faster than full-thickness joint degeneration. Peripheral nerve injuries usually take months for incremental recovery because axonal regrowth is slow. Muscle injuries typically improve faster than dense, low-vascularity tendons or ligaments. Clinicians tailor expectations to the tissue and disease stage — in advanced cases, combined or staged therapies plus guided rehab are sometimes recommended to maximize results.
Timelines vary because tissue biology, load demands, and baseline degeneration affect both onset and degree of improvement. Musculoskeletal clinics commonly track pain, range of motion, and activity tolerance as primary outcomes and use those measures to define milestones at 6–12 weeks and 3–6 months depending on the condition. The table below lists typical earliest improvements and functional milestones for common indications treated in regenerative medicine.
This comparison helps you set condition-specific expectations and prepares you for the knee, nerve, and sports injury sections that follow.
For knee osteoarthritis, many patients notice pain reductions within 6–12 weeks. Functional improvements — such as longer walks and easier stair climbing — tend to appear between 3–6 months as cartilage repair and joint remodeling progress. Clinicians track outcomes with pain scales and functional scores and often use a three-month follow-up to decide on additional or maintenance treatments. At NexGenEsis Healthcare we use mesenchymal stem cells (MSC), BMAC, and umbilical cord products along with image-guided delivery and staged rehabilitation to support predictable milestones. Patients with moderate-to-advanced disease can still see meaningful benefit, though timelines may be longer and staged plans are sometimes advised.
Peripheral nerve repair follows one of the slower timelines: sensory improvement or pain relief can appear in 1–3 months, while meaningful motor recovery often takes 6–12 months or more because axonal regrowth and remyelination are gradual. Sports injuries vary by tissue — muscle injuries usually get better fastest, with noticeable gains in weeks, while tendons and ligaments can take months to regain full tensile strength and sport-specific function. Return-to-play decisions are progressive and guided by objective strength and functional testing rather than fixed dates. Understanding this variability helps athletes and active patients set staged goals and plan a safe return to activity.
We find it helpful to frame the journey in four phases — Immediate, Incubation, Regeneration, and Long-term — each driven by different biology and patient experiences. Immediate effects reduce inflammation and ease symptoms. Incubation is when cells home and modulate the immune response. Regeneration brings structural repair and improved biomechanics. Long-term focuses on consolidation and preventing recurrence. Mapping common signs to each phase helps you and your clinician monitor progress and time any adjunct treatments. The list below summarizes the core signs and goals for each phase so you can recognize where you are in the recovery pathway.
Those phase markers lead into a closer look at what to expect in the first month and how regeneration unfolds over several months.
In the first 1–4 weeks after treatment, paracrine factors released by administered stem cells reduce cytokine-driven inflammation, which often produces early pain relief before structural changes occur. You may have local soreness at injection sites and some symptom fluctuation while immune modulation settles. Clinicians typically recommend activity modification and short-term symptom-directed measures. We also advise tracking progress with consistent tools — pain scores and daily activity logs — so your care team can tell whether recovery is on track. Understanding these early events sets realistic expectations for the slower regenerative phase that follows.
Starting around month two, structural and functional improvements become more measurable as tissue repair advances — examples include cartilage matrix production, tendon remodeling, and nerve remyelination. Range-of-motion tests, strength measures, and patient-reported outcome tools usually show steady improvement through months 2–6 and beyond. In select cases, imaging may demonstrate structural change. Rehabilitation is critical for translating biological repair into real-world function, and follow-ups at three and six months help determine whether additional treatments or maintenance biologics are needed. These long-term gains lead to stabilized function and an individualized maintenance plan.
You can help speed recovery and support durable results by following post-treatment plans that combine graduated activity, evidence-based rehabilitation, and lifestyle changes that reduce systemic inflammation. Typical protocols call for brief rest followed by guided physical therapy, weight management, sleep optimization, and smoking cessation. Select adjuncts — such as PRP, shockwave, or A2M injections — may amplify anti-inflammatory or reparative effects depending on tissue type and clinical judgment. The comparison table below summarizes onset and best-use cases for stem cell therapy, PRP, and A2M to help you and your clinician choose complementary strategies.
This comparison frames when each biologic may be most helpful and leads into concrete post-treatment actions you can take to support recovery.
For patients seeking anti-catabolic support in osteoarthritis, A2M injections provide a targeted option to manage symptoms and support joint health.
Following these steps helps shorten the path to meaningful milestones and lowers the chance of setbacks. The next section outlines specific post-treatment care measures.
Targeted post-treatment care — short activity restrictions, progressive loading through guided physical therapy, and selective adjuncts when indicated — creates the mechanical and biological environment that supports repair. Most providers recommend controlled range-of-motion exercises early, then progressive strengthening and sport-specific drills as tolerance improves, with regular monitoring to adjust the plan. Good sleep, glycemic control, and anti-inflammatory nutrition support cellular repair. Contact your clinic promptly if you notice red flags like increasing redness, fever, or uncontrolled pain. These care steps are practical ways you can influence both speed and durability of improvement.
Your habits and adherence to follow-up and rehab have a large effect on outcomes by influencing inflammation and mechanical stress on healing tissues. Smoking impairs microvascular supply and delays recovery; uncontrolled diabetes blunts repair; missed PT sessions reduce functional gains and lengthen timelines. Measurable lifestyle changes — quitting smoking, improving sleep, optimizing body weight, and committing to therapy — can materially shorten the time to activity milestones and improve long-term results. Honest communication with your care team about barriers lets them tailor support to keep you on track.
Real-world patient data and anonymized clinic summaries provide useful context for expected timelines and outcomes, but interpreting success rates depends on who was treated and how success is defined. Observational reports commonly show meaningful pain reduction and functional improvement in many patients within 3–6 months; however, randomized trial evidence is still developing for some indications. Clinic-reported materials sometimes show high success in carefully selected populations — for example, some materials cite a 90 percent success rate for moderate-to-advanced arthritis and multi-site degeneration when patients are selected and treated with a comprehensive protocol. The table below summarizes common outcome metrics clinicians use and what those measures mean for patients.
Putting these metrics alongside clinic-reported outcomes helps set realistic expectations. Below are anonymized case themes that illustrate typical timelines.
Anonymized case summaries commonly show a pattern: early pain relief within weeks, stepwise functional gains over 3–6 months, and continued improvement through six months that influences decisions about further care. Patients often report decreased reliance on pain medications early and better walking tolerance and daily activity by three months, with some returning to higher-level recreational activities later as strength and endurance improve. There’s natural variability — some improve quickly, others need staged interventions — so clinicians emphasize tracking individualized milestones rather than rigid deadlines. These patterns support a shared decision-making approach where progress is measured and plans are adjusted.
Success for chronic joint pain and arthritis depends on patient selection, the biologic used, image-guided delivery, and comprehensive rehabilitation. When those elements align, observational data and clinic reports show meaningful symptom relief and functional gains for many patients. As noted in clinic materials, NexGenEsis Healthcare reports a demonstrated 90 percent success rate for moderate-to-advanced arthritis and multi-site degeneration in selected patients treated with a structured regenerative protocol. It’s important to interpret such figures in context: “success” may mean meaningful pain reduction, improved function, or delaying joint replacement rather than full disease reversal. For a personalized prognosis and to discuss whether a regenerative pathway is right for you, schedule a consultation with NexGenEsis Healthcare to review options and timelines.
Stem cell therapy is generally well tolerated, but you may experience temporary soreness at the injection site, mild swelling, or bruising. Rarely, allergic reactions or infections can occur. Discuss risks with your provider before treatment — they’ll review concerns based on your medical history and the specific product we plan to use.
Yes. Research is exploring stem cell use beyond joint pain — in certain neurological conditions, heart disease, and select autoimmune disorders. Results vary by condition and individual factors, so a specialist consultation is essential to determine whether stem cell therapy is a reasonable option for your specific issue.
Candidacy requires a thorough evaluation by a qualified provider. We consider age, overall health, severity and duration of the condition, and prior treatments. Diagnostic testing and a detailed medical history help determine suitability. If conservative care hasn’t worked, a personalized consultation will clarify whether regenerative treatment is appropriate.
Small lifestyle changes deliver big benefits. Eat an anti-inflammatory diet, stay hydrated, prioritize sleep, and follow your prescribed exercise plan. Avoid smoking and manage stress. Adhering to a structured rehab program and following medical advice optimize healing and long-term results.
Follow-up schedules vary by treatment and condition. Generally, we see patients within the first few weeks to check progress and adjust rehab. Additional visits commonly occur at 3, 6, and 12 months to assess longer-term outcomes and discuss any further interventions. Regular communication keeps recovery on track.
Yes. Rehabilitation is a key part of success. Protocols usually begin with gentle range-of-motion exercises shortly after treatment, progressing to strengthening and functional activities as tolerated. The exact plan depends on the treated area and your goals. Working with a physical therapist familiar with regenerative care ensures rehab is tailored to your needs.
Understanding the healing timeline for stem cell therapy helps you set realistic expectations and take an active role in recovery. Recognizing the phases of healing and the factors that influence outcomes lets you and your care team optimize treatment and reach meaningful functional gains. For personalized guidance and to explore your treatment options, schedule a consultation with our team — take the next step toward better function and quality of life.
Don’t let chronic pain hold you back. Our expert team at NexGenEsis Healthcare San Antonio is ready to provide personalized guidance and explore your treatment options for relief.