
Stem cell therapy is an increasingly used option for people living with chronic pain when standard treatments aren’t enough. This article lays out a practical timeline for results and explains what typically happens during recovery. Knowing how the treatment works and which factors shape outcomes helps set realistic expectations—whether you’re managing osteoarthritis, back pain, or neuropathy. We’ll walk through a typical timeline, what can speed or slow progress, and how to get the most from this approach.
Our expert team at NexGenisis Healthcare Columbus is dedicated to providing personalized stem cell therapy. Schedule a consultation today to discuss your options.
Stem cell therapy is a form of regenerative medicine that uses the body’s own healing cells to encourage repair and reduce inflammation. Rather than simply masking symptoms, these cells release growth factors and signaling molecules that calm inflammation and support tissue repair. In many cases the benefit comes from those paracrine (cell-to-cell signaling) effects more than from the cells turning into new tissue themselves.
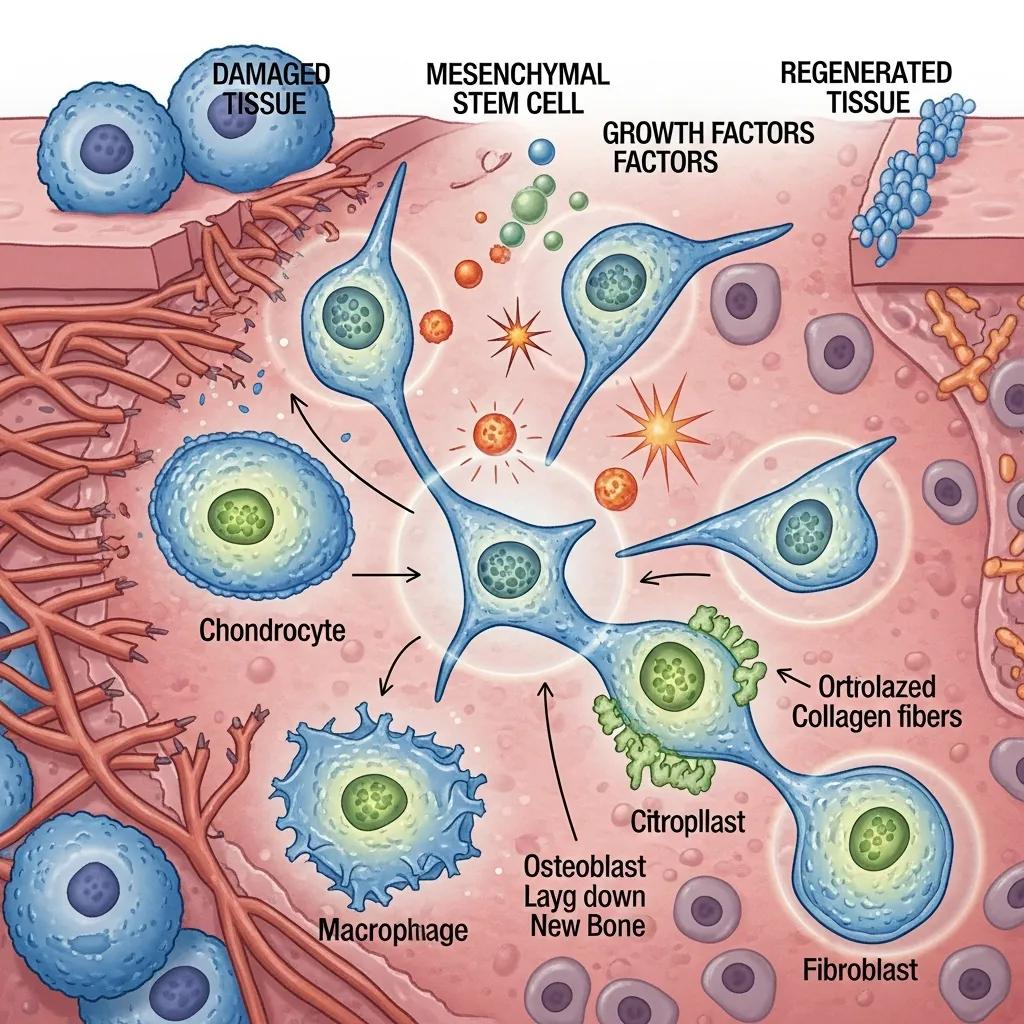
Mesenchymal stem cells (MSCs) are commonly used because they can both adapt toward cartilage, bone, or muscle cells and secrete compounds that lower inflammation and promote healing. In conditions like osteoarthritis, MSCs can help change the joint environment and encourage cartilage preservation and repair, which often translates to reduced pain and better function.
Clinically, a few stem cell approaches are most common:
Treatments are selected and customized based on the patient’s condition and goals to improve the chances of meaningful pain relief.
Recovery and results vary by person and condition, but most patients follow a recognizable pattern. Below is a general timeline to help you understand what to expect.
Ongoing research continues to refine timelines and improve the techniques used in regenerative treatments.
In the first one to two weeks you may notice mild soreness, swelling, or bruising around the injection site. These reactions are normal and usually short-lived. The body is beginning its early response, but most people don’t see major pain relief during this phase.
Between weeks three and six some patients report gradual reductions in pain and slight gains in mobility as inflammation drops and early repair processes begin. Responses vary—some people feel helpful changes sooner, others later.
By two to three months many patients notice clearer improvements in pain and function. This is when tissue modulation and regeneration often become more apparent, and day‑to‑day activities can feel easier for many people.
From four months onward improvements frequently consolidate and can continue to progress. Some patients experience durable relief lasting months to years. Long‑term results depend on the treated condition, overall health, and follow‑up care—so regular check-ins with your provider are important.
Several variables influence recovery speed and overall results. Understanding them helps set realistic expectations.
The more advanced the tissue damage, the longer it usually takes to see benefit. Joints, discs, nerves, and soft tissues all respond at different rates, so recovery timelines differ by treatment area.
Younger, healthier patients often see faster improvement, and following your post‑procedure plan—physical therapy, activity guidance, nutrition and sleep—can significantly improve outcomes. Commitment to rehab and lifestyle adjustments supports the healing process.
Stem cell therapy has shown encouraging results across several pain conditions. Below are typical expectations by condition.
Many knee osteoarthritis patients begin noticing reduced pain and better mobility within 4 to 12 weeks after treatment. Individual responses vary, but clinical data support meaningful improvements for many patients.
Clinical studies have consistently reported positive effects of MSCs on pain and function in knee osteoarthritis.
For back pain and degenerative discs, some patients see early improvements within 1 to 3 months, with more pronounced benefits possibly developing over several months. Consistent follow‑up and targeted rehab help optimize outcomes.
Shoulder and hip conditions often show gradual relief, with many patients noticing changes in 6 to 12 weeks and continued improvement afterward as tissue healing and functional gains accumulate.
Neuropathy responses are more variable. Some people report symptom relief within weeks; others require months. The goal is to support nerve recovery and reduce pain over time—results depend on the underlying cause and treatment plan.
There are practical steps you can take to support healing and improve the chances of a good outcome.
Simple, consistent habits help your body make the most of regenerative treatments:
Adhering to your provider’s guidance on activity, physical therapy, and any prescribed medications is critical. Skipping recommended rehab or returning to high‑risk activities too soon can delay recovery or reduce benefit.
This table summarizes typical outcomes and timelines for common conditions treated with stem cell therapy and highlights the realistic benefits many patients experience. If you’re exploring advanced pain solutions, NexGenisis Healthcare offers tailored regenerative treatments.
Stem cell treatments are generally well tolerated, but some patients experience short‑term soreness, swelling, or bruising at the injection site. Rare but possible complications include infection, bleeding, or allergic reactions. We recommend discussing risks and safety with your clinician so you understand what to watch for before and after treatment.
Traditional treatments like NSAIDs or injections often focus on symptom relief. Stem cell therapy takes a regenerative approach, aiming to address tissue damage and chronic inflammation—potentially offering longer‑lasting improvement rather than temporary symptom control. The best option depends on your diagnosis, goals, and overall health; your provider can help you weigh choices.
Yes. Stem cell therapies are being studied for a range of conditions, from degenerative joint disease to certain autoimmune and neurological disorders. Evidence and regulatory approvals vary by application, so consult a specialist in regenerative medicine to understand current, evidence‑based uses.
Expect a thorough review of your medical history, symptoms, and prior treatments. Your provider will explain potential benefits and risks, discuss realistic timelines, and may order imaging or tests to assess severity. The goal is a personalized plan that fits your condition and goals.
Coverage varies. Many insurers consider certain stem cell procedures investigational and may not cover them. Check with your insurance company and discuss financial options with your clinic to understand potential out‑of‑pocket costs.
Regular follow‑up visits are the best way to monitor progress. Providers will assess pain, mobility, and function over time. Keeping a symptom journal—notes on pain levels, activities, and improvements—can help guide adjustments to your care plan.
Stem cell therapy represents a regenerative option for people seeking more than short‑term symptom relief. By understanding the typical timeline, the factors that influence healing, and the steps you can take to support recovery, you’ll be better prepared for the road ahead. If you’re considering regenerative treatment, our team is available to answer questions and build an individualized plan that fits your needs. Take the next step toward lasting pain relief by reaching out to learn more. Discover how NexGenisis Healthcare Columbus can help you achieve lasting pain relief.